Want to know the secrets of an emerging scientific field that could help you conquer sugar cravings, lose weight more effectively and enhance your mental health?
The answer lies in your gut.
You probably don’t spend a huge amount of time thinking about your food after it passes your mouth. But there is a tonne of evidence showing that the digestive system and the microbial ecosystem it hosts are major players that influence everything from body composition to hunger, your mental well-being and many more.
If you’re interested in maximising your physical and mental well-being, making your microbiome the star of the show could be just the trick you didn’t know you needed.

What is gut health?
Think that gut health is all just about bacteria? Not quite.
Gut health broadly refers to the optimal functioning of the digestive system. But you’ll feel the effects of your digestive system start before food even touches your lips.
We all know what it’s like to start drooling when we walk past a bakery and encounter the irresistible aromas of a freshly baked loaf or fluffy croissant. From the moment we even think about or anticipate food, the body starts to produce saliva, which contains enzymes that break down foods and make it easier for the body to digest them.
But there’s far more to it than that.
You could be forgiven for thinking that the digestive system’s only role is to process and harvest energy from food. You may not have realised that it’s one of the immune system’s major lines of defence.
And the body has a very clever way of keeping harmful nasties at bay. Your gastrointestinal tract is lined by a mucus layer that contains 70-80% of the body’s immune cells [1]. This layer is designed to trap foreign and pathogenic substances in this mucus and weed them out.
And if you thought your digestive system just took up some important internal real estate, that’s where you’d be wrong.

The gut-brain axis
You might have thought that your stomach and brain don’t have much to do with one another but in fact, they are effectively one and the same.
Your gut has a direct line of communication with the brain, a pathway known as the gut-brain axis.
Through the vagus nerve, which links the brain with the gut, this gut-brain axis shares information about everything from hunger, fullness, blood glucose levels, stress, mood, and sleep levels.

Why your gut is running the show
Ever wondered why you can’t just have one bit of chocolate? Think back to the last time you indulged your sweet tooth. Chances are, you probably found yourself craving more.
So, what’s going on here? The answer is in your gut…
We now know that the GI tract is home to a network of what are known as ‘neuropod cells’.
These cells send rapid signals that tell the brain whether foods contain things like sugar or salt (that our body deems vital for survival), these neuropod cells then stimulate us to eat more [2].
Believe it or not, your gut can also detect whether that soda you just drank was a full-sugar or a diet version through its ability to detect energy [3].
And this makes perfect sense from an evolutionary perspective. As humans, we are designed to withstand periods of food scarcity. But in today’s modern food environment, where the mere click of a button gives us access to thousands of calories that can be consumed in minutes, this mechanism could be driving us headlong towards obesity.

What is your microbiome and why is it important?
Believe it or not, you have around 38 trillion microbial cells in your gut. These bacteria, which act as a kind of symbiotic organism within us, contain a whopping 150 times more genes than the human genome.
But what’s this got to do with your mental health? Everything!
Gut bacteria are constantly evolving based on what you feel and do, and what you put in your body.
It’s not uncommon for periods of high stress to result in changes in your digestion, such as bloating or gas. You might also experience sensitivities to certain foods. This is a prime example of your digestive system and gut bacteria adapting in response to your environment.
Gut bacteria can even change the location of key chemical markers throughout the human genome, which may help to fight infections and prevent cancer. And while there’s a lot we can do to create a healthy microbial environment, there is also a strong genetic component to the make-up of your gut bacteria and how it reacts to various stimuli [4].

How does the microbiome form?
We actually inherent a large proportion of our microbiome from our mothers. From the very moment we are born, our immune systems start to interact and develop symbiotically with this gut flora [5],[6].
This part of our development is so important that doctors and researchers are focused on it as early as the delivery room.
Babies born via c-section miss a critical stage that may put them at increased risk of developing obesity and asthma in later life [7],[8]. Researchers believe that this is because infants gain their microbiota through contact with maternal vaginal fluid.
In a crucial breakthrough, researchers have explored the effect of applying vaginal fluid to newborns. The early results show that this restores the microbes babies miss from surgical delivery. And while this practice remains at an experimental stage, it is an exciting new development in disease prevention [9].
So how does our microbiome shape our mood and mental health? Here’s where it really gets interesting.

How does gut health affect your mood?
Evidence indicates that our gut microbiota can directly influence an area of the brain known as the HPA (hypothalamic-pituitary-adrenal) axis. And while this may sound like some hardcore science, it’s a change that can have a domino effect on your metabolism, hormonal health, and the body’s stress response [10]. Small interruptions to this system can therefore have a butterfly effect on how you feel, think, and react in everyday life.
Nothing illustrates this concept better than what some researchers are doing to turn the tide on obesity.
Early data shows that faecal transplants (yes, that is a poo transplant) could help to treat a range of lifestyle diseases [11]. Granted, you probably won’t be rushing to the doctor to ask for a hefty dose of someone else’s dark matter. But the results in both animal and human models have provided positive early indications.
The process involves transferring microbial samples from healthy, lean patients to obese subjects. And what we can see in patients who have undergone this treatment is that their bodies are better able to process carbohydrates, indirectly leading to weight loss [12], [13]. It’s still early days, but it might not be long before a stool transplant becomes a mainstream tool in the fight against fat.
Elsewhere it has also been shown that improvements in digestive health can aid weight loss through improved absorption of nutrients and appetite management [15], [16]. And if you’re not quite chomping at the bit to start eating someone else’s poop, keep on reading to learn quick and easy tips you can apply today to reap the benefits regardless.

Is leaky gut affecting your mental health?
By now, you’re probably thinking that’s all there is to it when it comes to the link between your gut and mood.
Think again…
The intestinal barrier or epithelium covers a surface area bigger than the average IMAX cinema screen and accounts for up to 40% of your body’s energy expenditure [17]. This massive sensory organ is a key player in managing our mental health.

You may have heard of a condition known as ‘leaky gut syndrome’.
Now, this doesn’t mean you need to call the out-of-hours plumber…
It refers to a condition where the connections between the cells lining the GI tract become permeable, allowing undesirable compounds to enter the body. This can send the body’s protective inflammatory mechanism into overdrive, reducing the body’s ability to perform optimally and increasing the risk of everything from Alzheimer’s to various forms of cancer [18], [19]. Stress, in particular, is one of the key triggers of this negative chain of event [20], [21].
And while the name might bring a smile to your face, leaky gut’s effects aren’t a laughing matter.
Leaky gut, also known as intestinal permeability is associated with numerous disorders, such as IBS, rheumatoid arthritis, Alzheimer’s, asthma, autism spectrum disorders, and low-level inflammation seen with metabolic syndrome, obesity and diabetes [22].
But there’s good news.
A very special type of food can solve all these problems.

Feed your good bacteria
The solution is not the latest ‘gut-friendly’ wheatgrass, organic, gluten-free, small-batch health shot.
It’s actually found in the vegetable drawer in your fridge.
When we eat plant-based foods, they are broken down via fermentation in the final stage of digestion in the large intestine. One of the products of this process are short-chain fatty acids (SCFAs) and they are critical to maintaining our physical and mental well-being [23].
One of their most important roles is to maintain the integrity of the intestinal barrier, producing that all-important immune-boosting mucus and protecting against inflammation [24].
SCFAs also crucially help control levels of neurotransmitters such as dopamine and serotonin, chemicals that regulate motivation, feelings of happiness and reward [25]. Think more veg, less stress!
Now, based on the above, you might think your digestion is in top form.
But if you’ve even stepped out from under a rock recently, chances are your happy bacteria could be upset by something.
Is your lifestyle affecting your gut health?
In today’s modern world, we are exposed to a myriad of substances and experiences that can disrupt the delicate ecosystem inside us.

High stress, processed foods, antibiotics, chemical compounds in our environment, food, and even beauty products can all trigger minute changes that upset this balance. This condition is known as dysbiosis, and it is far more common than you might realise.
Everything from minor issues like dandruff or dandruff or psoriasis right through to PCOS or alopecia could be a sign that your gut bacteria are off kilter [26], [27].
And its effects aren’t just physical. Many mood and behavioural disorders, like anxiety, depression, autism, chronic fatigue, bipolar and many more, can also be traced back to dysbiosis [28], [29].
How is your gut health?
So, how can you tell if your gut health is in tip-top condition?
As you’ve probably guessed, your digestive system is pretty complex. This means that it’s generally very difficult to pinpoint the source of problems without laboratory testing. So, if you think things aren’t right, do seek professional medical advice.
But we also have a couple of tools up our sleeve that you can use right now to assess your gut health.
The Bristol stool chart describes the typical composition of different types of stool, based on colour and consistency.
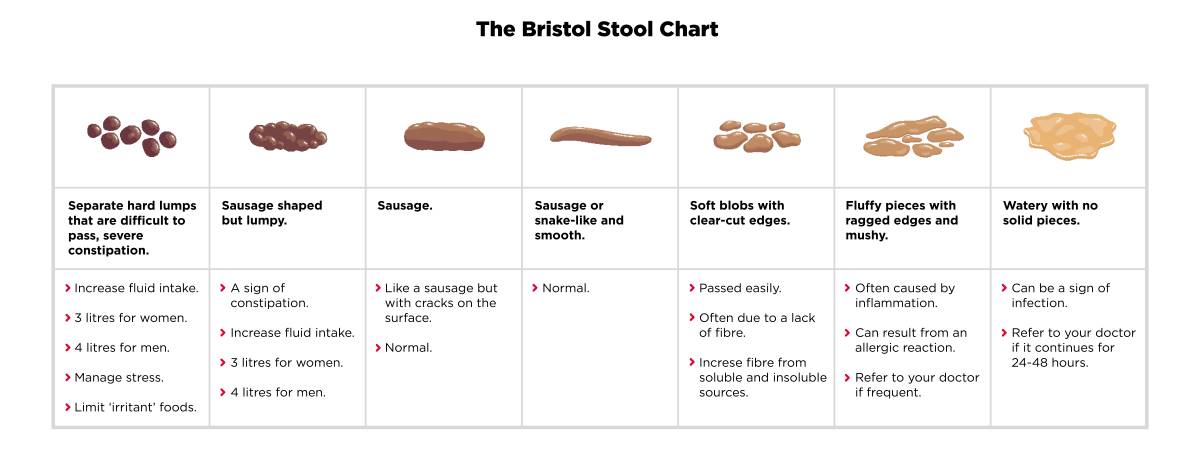
If you’re normally somewhere in the middle of the chart, you’ve got yourself some top-rated poop. But if you rarely experience what is considered ‘normal’, you likely need to make some lifestyle changes.
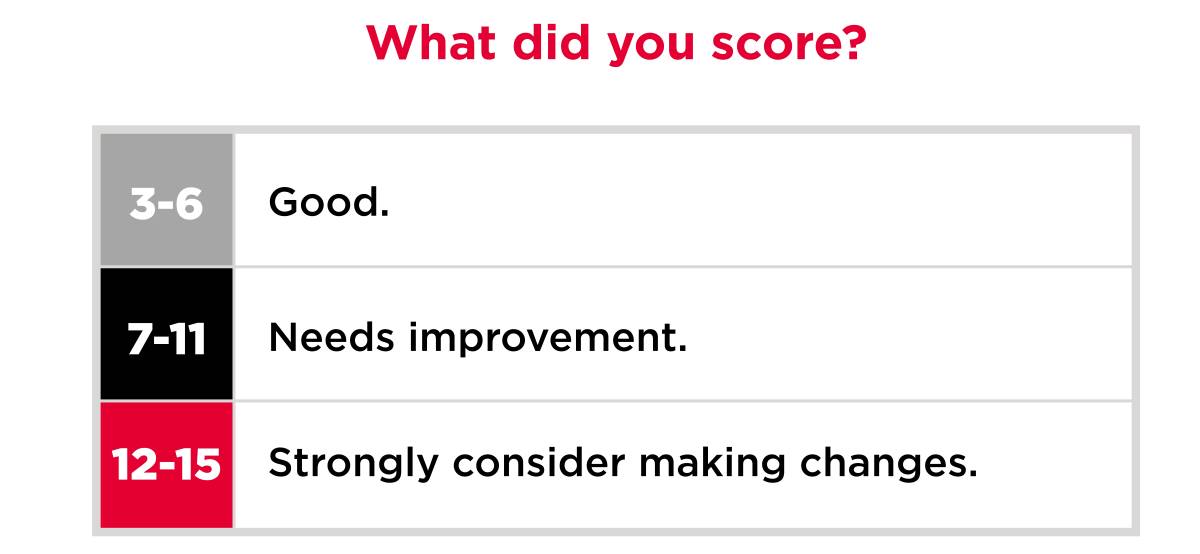
Many of us also aren’t very good at telling whether our gut health is optimal. Our gut health quiz below is perfect for a quick check-up.
How often do you feel digestive discomfort, such as bloating or abdominal cramping?
- Never
- Sometimes
- Often
- Mostly
- Always
Does this comfort or pain for once you’ve had a bowel movement?
- Never
- Sometimes
- Often
- Mostly
- Always
How often does digestive pain or discomfort impact your daily life, such as sleep or concentration at work?
- Never
- Sometimes
- Often
- Mostly
- Always
8 tips to build a bullet-proof gut
Hopefully, we’ve won you around that your gut warrants some TLC. But if you’re not sure where to start on making a change, we’ve got some easy to apply tips you can use today.
1. Take your time when eating to improve your gut health
Chewing is the first stage in the digestive process, which reduces workload later down the chain. Make sure to chew for at least 30 seconds with each mouthful.
2. Manage stress to improve your gut health
Whether it’s taking time out for a hobby, yoga, meditation, guided breathing or whatever works for you, build stress management into your routine so you can stay on top of it before it starts wreaking havoc.
Before eating, it is also useful to move into a parasympathetic (relaxed) state. Try listening to calming music, performing breathing exercises, and avoid eating at your desk.
3. Track your food intake to improve your gut health
Keep a food diary and note down symptoms, such as bloating, gas, heartburn or changes in frequency of bowel movements. This will allow you to pinpoint trigger foods to either cut them out for a time or phase them back in gradually when symptoms improve. Only perform an ‘elimination diet’ under medical supervision.
4. Eat as many vegetables as possible to improve your gut health
Vegetables provide the nutrients that feed your microbiome and help to produce neurotransmitters. An easy rule of thumb is to ensure that at least half of every plate is full of vegetables. Think ‘eat a rainbow’!
5. Prioritise high-quality sleep to improve your gut health
Our natural circadian rhythm plays a crucial role in regulating processes such as digestion, and when it falls out of sync, this can also disrupt your natural rhythm. Daylight exposure during the day and putting away electronic devices after dark are important to maximise sleep quality and keep your body in alignment.
6. Feed your gut to improve your gut health
Certain foods, such as prebiotics and probiotics, provide the right environment for your microbiome to thrive. Probiotics provide bacterial seed populations that may be missing, while prebiotics help support your microbiome by feeding healthy bacteria. Think kefir and cultured yoghurts; pickled foods such as sauerkraut, gherkins or kimchi are also tasty options.
7. Hydrate to improve your gut health
Water is vital for the effective functioning of the digestive system, so make sure to set yourself reminders if this is a challenge. In general, men should aim for around 3.7 litres per day and women 2.7 litres.
8. Use supplements to support positive diet and lifestyle changes
Supplements should never replace a healthy diet and lifestyle, but they can be highly beneficial for improving gut health by improving the absorption of nutrients and encouraging a healthy microbiome.

5 key supplements to give your gut health a boost
Pre-Bio Fibre
Besides providing bulk to stools, fibre provides nourishment for the healthy bacteria in the gut. Drink plenty of water with fibre. The perfect assistant if you struggle to up your fibre intake through fruit and vegetables.
Gut Flora
Provides seed populations of healthy bacteria. These bacterial populations use fibre and other nutrients in our diets to flourish and are good for overall health and body composition.
Glutamine powder
Glutamine is the primary source of energy for the cells lining the gut. If you have a very stressful lifestyle, have previously taken antibiotics or had an unhealthy diet, glutamine powder is a must to help keep your gut in good working order.
Digestive enzymes
Provides natural digestive enzymes to fortify those produced by the body to ensure you have sufficient levels for thorough digestion as your digestive system begins to heal.
Longvida curcumin
Curcumin works as a potent anti-inflammatory, which helps to reduce and prevent symptoms associated with digestive issues caused by a bad diet or food intolerances.
To purchase these supplements, head to our online store.
Please check with your clinician before taking any new supplements.
The take-home
- You could be forgiven for not feeling electrified at the thought of your gut health. But if you’re serious about optimising your physical and mental well-being, it’s an area you can’t afford to overlook.
- There can be several complex causes behind digestive problems, so if you are suffering, speak to your doctor, who will be best placed to advise.
- But with these simple tips, you can take back control, helping you to feel more energised, invigorated and happier to boot.



