Welcoming a baby into the world is, of course, a joyous event. But along with it comes a host of new challenges; emotional and physical shifts, juggling nappy changes, baby feeds and chores, trying to take care of yourself, all on minimal sleep.
With so much going on, it’s hard to find time to focus on yourself and get back to your health and fitness goals.
But in this quick-start guide, find you everything you need to navigate the challenges of a new baby.
We cover everything from getting back to exercise, nutritional pointers, and lifestyle tips you can apply today to help get you through the post-partum period.
How soon can you start exercising?
There are all kinds of conflicting advice from both healthcare providers and online about the ‘safest’ time to resume training. The general clinical recommendation is to wait at least four to six weeks post-partum before doing any intense exercise.
However, the truth is that whether and when you choose to start exercising again is highly individual and depends on the type of birth. For instance, did you have a vaginal birth or a c-section? Do you have significant diastasis recti or stretching of the linea alba? Did you have any complications during your pregnancy? What kind of training did you do before and during your pregnancy? All these factors affect how quickly you can return to training and what form that takes.

Shilpa got back to training after having a baby to feel amazing again.
Why do doctors recommend waiting before resuming exercise?
The process of growing and giving birth to a baby involves a series of major physical changes, and your body needs time to heal. This is even more important if you had a c-section. C-section deliveries involve cutting multiple layers of tissue and suturing them back together; it’s a major operation, and you will need time to heal.
Whether your birth was natural or otherwise, your abdominal muscles are stretched and weakened, or you may have needed treatment for problems like a vaginal laceration (which may require stitches). Don’t feel like you have to rush back into training to return to your pre-baby body as quickly as possible. Returning to intense exercise too soon could increase the risk of:
- Bleeding
- Infection
- Muscle injury
- Joint injury
- Back pain
Women are at increased risk of injury post-partum due to the influence of relaxin, a polypeptide hormone that the body releases during the first trimester to allow the stomach to expand. It also increases laxity in the sacroiliac joint to accommodate the growing baby[1]. Relaxin may continue to circulate for several months after birth, so you may find it harder to brace, or your joints may not feel as stable.
However, if you take your time and are careful, there’s no reason you can’t start reincorporating some form of movement within the first few weeks after birth (if you feel up to it). Make sure you have medical clearance from your doctor to exercise, and always pay close attention to how you feel.

The benefits of post-partum exercise
Pregnancy brings about huge changes in your body, and many women feel immense pressure to get their ‘pre-baby body’ back. Of course, maintaining a healthy body composition is important for you and your baby throughout your pregnancy and beyond[2]. But the focus at this time doesn’t need to be pressuring yourself to fit into all your old clothes or hitting a certain weight goal. If you can manage to do any movement or have time to eat a nutritious meal during this time, you’re doing great!
We do know, however, that post-partum exercise has several benefits for new mums, including:
- Improved cardiovascular fitness
- Weight loss
- Increased positive mood
- Decreased anxiety
- Decreased risk of postnatal depression
What exercise can you do in the first six weeks?
Even if you don’t have the all-clear from your doctor to resume training in full, there are still things you can do to start the recovery process. Three forms of activity you can do in the first few weeks include:
- Walking
- Rebuilding your core
- Strengthening your pelvic floor muscles
If you’re concerned about going overboard, remember that your body will let you know if you are exercising too much. It’s completely normal to experience some unusual pains while performing everyday talks and generally feel tired. So, before you start exercising, make sure to follow these five guidelines:
- Do not start exercising without first speaking to your doctor or midwife
- Wait until any pain has gone
- Wait for any bleeding to stop
- Pay attention to joint pain or discomfort and stop if it persists
- Keep hydrated. Water is vital both for your bodily processes and producing milk for your baby
Vaginal bleeding or lochia is common after giving birth but if you need to use more than one pad per hour, speak to your doctor.

The first six weeks
It’s unlikely that you’ll want to go in all guns blazing after giving birth, but when you are ready to start moving, here are three key exercises you can start with. You may be happy to try exercises one and two in the days after giving birth, but it’s ok to wait if you don’t feel up to it yet.
(With all three exercises, make sure to double-check with your doctor health visitor first).
Focus on improving your breathing and core stability
Your core comprises much more than just your ‘abs’ and includes your diaphragm, the multifidus (which support the lumbar spine), your pelvic floor and your abdominals. Together, these muscles form a box that gives you stability and holds you upright. However, given that they’ve probably been pushed to their limits through pregnancy, it may take some time to regain their former strength.
Learning how to gain and release tension in your abdominals and pelvic floor will help you regain control of these muscles and connective tissues.
- Start in a lying or side-lying position. If you want to progress the exercise, try sitting; standing is the hardest position.
- As you inhale, it should feel like your ribcage, stomach, and the base of your pelvis are gently filling up with air like a balloon.
- As you exhale, think about breathing the air outwards from your ribcage, stomach and the base of the pelvis.
- Repeat for two sets of ten breaths daily.
Half-kneeling hip flexor stretch and overhead reach
This movement helps you improve your stability and provides a nice stretch through the diaphragm and ribcage.
- Start in a short lunge stance on the floor, with both knees at a 90-degree angle.
- Make sure to spread your weight evenly through both legs but with a slight emphasis on your back leg.
- Squeeze the glute on your back leg and focus on creating a stretch through your hip flexors and quadriceps.
- On the same side as the knee that is on the floor, reach up and stretch your arm in the air, reaching as far as you can with your fingertips. To open the ribcage further, lean over the front leg.
- Repeat the movement on each side, performing two sets of six to eight reps daily.

Bodyweight glute bridge
The glute bridge uses the glutes, hamstrings and quadriceps but also requires stabilisation from your core muscles.
- Start by lying on your back on a mat, bending your knees so that your feet are flat on the floor.
- Inhale and focus on keeping your tailbone, spine and head aligned throughout – imagine a ruler running from your tailbone to the top of your head.
- Raise your hips in a bridge position, squeezing your glutes as you move.
- Stop at the top when you can go no further without arching your back.
- Lower slowly to the floor and maintain the ruler along your back, making sure your lower back does not hyperextend.
- Repeat for three sets of 10-12 reps daily.

Exercising after a vaginal birth
If you want to start moving, you can begin the three exercises above within the first day or two after birth but stop if you feel any pain.
Going for a gentle walk is a good way to get out with baby and get some light steps in when you feel ready. You don’t have to be manic about hitting a step count but start at around ten minutes a day and try to build up to a daily 30-minute walk.
However, avoid swimming until any bleeding has stopped for at least seven days and you’ve had your postnatal check-up with your doctor or midwife (normally six to eight weeks post-partum). You should also wait for the medical all-clear before you go back to the gym. Generally, clinicians recommend waiting around 16 weeks before returning to your previous activity levels.
Exercising after a C-section
A caesarean is a significant operation and represents a major stress on the body. As a result, it’s important to take your time and give your body time to heal. Normally, this is at least six weeks. That being said, you can start pelvic floor and breathing exercises from the first day after birth (if you want to). However, it’s important to avoid sit-ups, crunches or any exercises that put pressure on the scar or cause your stomach to dome or bulge. Depending on your recovery, you may need to avoid any high-impact exercise for around three to four months after your caesarean.
During the first six weeks, avoid lifting anything heavier than your baby, making sure to hold the baby close to you to prevent any additional strain. It’s also a good idea to keep daily supplies and food close to you, so you have everything in easy reach. During the first few weeks, if you cough or sneeze, make sure to hold your scar to protect the incision site.
However, if you feel up to it, there are still some safe forms of exercise you can do in the days after having your baby.
Abdominal bracing
You can use this alongside the breathing exercise above.
- Starting sitting down, standing, lying on one side, on your back or all fours.
- As you take in a deep breath, focus on drawing in as much air as possible and expanding the ribcage.
- As you breathe out, focus on expelling the air as if you’re threading through a needle, pulling your belly button in towards your spine.
- Once you’ve drawn it in as far as you can, hold for 5-10 seconds, breathing normally.
- Repeat 8-12 times, four times a day.
Pelvic floor exercises
- From a sitting position, focus on squeezing and lifting your pelvic floor towards your diaphragm. This should feel like the sensation you experience when you are trying to stop yourself from urinating.
- Once you have contracted the muscle, count to eight or as long as you can hold for, then relax for eight seconds before repeating a further 9-11 times (total of 8-12 reps).
If you are still leaking urine three months post-partum, speak to your doctor, who will be able to recommend further support for strengthening your pelvic floor.
Likewise, if you find it difficult to empty your bowel or bladder, feel a sense of pressure in your vagina or notice a bulge or swelling in your vagina, you could have a prolapse. Speak to your healthcare provider, who will be based placed to advise you.
If you’re still experiencing pain, ask your doctor, who can advise on what types of pain relief you can take, especially if you’re breastfeeding.

Exercising after six weeks
Before you move on to any high-impact exercise, make sure you have the all-clear from your doctor or midwife to do so. It’s also important to check whether your pelvic floor is ready. A simple test is to cough or jump with a full bladder to see if you leak urine. If you don’t, you should be ok to exercise.
Exercising with diastasis recti
Diastasis recti refers to the stretching of the linea alba, the connective tissue that connects the rectus abdominis or ‘six-pack’. This is a completely natural process that allows the abdomen to expand during pregnancy. It is estimated that up to 100% of pregnant women experience diastasis recti[3]. And research shows that up to 60% of women still experience diastasis six weeks post-partum. Figures indicate that this ranges from mild diastasis (two fingerbreadths) to severe (more than four fingerbreadths)[4].

After giving birth and your uterus returns to its pre-baby size, the linea alba should return to normal. However, in some circumstances, depending on genetics, improper breathing and movement mechanics, it may become overstretched and fail to return to its previous state.
Determining diastasis recti
If you believe you have diastasis recti, see your doctor for medical confirmation. However, there are a couple of quick home tests you can do.
Starting from a lying position, gently press two fingertips down the centre line of your stomach from your ribcage to the top of your pubic bone. While your abdominal muscles are relaxed, check to see if you feel any difference in the tension between the muscles. If there is a spot where there is less tension, or it feels like a hole or dip, you may have diastasis.
From this same lying position, place one hand behind your head and focus on lifting your head, neck and shoulders an inch off the ground, focusing on drawing your ribcage and pelvis together. If you notice a bulge in your stomach, this could also indicate diastasis. However, perform step one again and feel for any loss of tension. If you feel a dip or hole, you can test for its width using your fingers.
If you’re not sure if you have diastasis, but you often experience back pain, constipation, bloating, poor posture or find it harder to contract your abdominal muscles, speak to your doctor, who will be able to recommend suitable support services.
Exercises for diastasis recti
While you should avoid anything that causes your stomach to bulge or dome, such as crunches, there are other effective core exercises you can incorporate to start the healing process
- Start by lying on your back. Aim to pull your sternum down towards your belly button, ensuring that there is no space under your lower back.
- Keep this position throughout the whole movement. In this position, you should feel your core contracting.
- From here, bring your feet off the ground till your knees are in line with your hips. Your arms should be raised in front of you, so the wrist and elbows are directly over the shoulder. This is your start position.
- Straighten one leg out in front of you and simultaneously straighten the opposing arm out behind you before raising into the start position and performing it with the opposing side.
Palov press
- Start with a cable set at the same height as the bottom of your ribcage with a d-handle on one end. Stand so that you are perpendicular to the machine with the cable coming across your body.
- Move far enough away from the stack so that there is tension on the cable.
- Keeping your feet and hips fixed (don’t allow them to rotate), bring the cable across to the midline of your body, pause and then extend the arms outwards so that your arms are fully extended in front of your chest.
- Hold this position and resist the pull of the cable to draw you back towards the machine.
- After 5-10 seconds, bring your hands back to the centre.
- Perform all your reps on one side before turning with your other side to the machine and repeating on that side.
If you want to progress the exercise, adopt a narrower stance. Reducing your base of support means your core must work much harder to keep you stable.

- Lay on to your side with one foot on top of the other.
- Rest your elbow on the ground, ensuring that it sits directly under your shoulder.
- Raise your whole body off the ground keeping contact at only two points – the feet and the elbow.
- Don’t allow your hips to drop as you fatigue.

Post-partum nutrition: focus on nutrients not calories
Having a baby is an experience that comes with a swirl of new emotions, stresses and time demands, so don’t feel like you have to nail your nutrition straight away. The aim at this time should be to eat in a way that supports your recovery and allows you to provide your baby with the love and care he or she needs. If you can even find time to eat a good meal right now, this is a huge win!

Post-partum calorie requirements
Your calorie requirements after giving birth depend on whether you breastfeed, your body composition and your general activity levels.
If you are not breastfeeding, your nutritional requirements are unlikely to be vastly different to before pregnancy if your body composition has not changed significantly.
For most women who are breastfeeding, your daily calorie requirements may not change too much. While nursing may burn around 450-500 calories per day, keeping your calorie intake similar to pre-pregnancy levels is sufficient to provide plenty of nutrients for your baby as well as aid in weight loss. If you are not trying to lose weight, you may need to increase your calorie intake to match your output.
Focus on maximising your nutrient density
In the immediate post-partum period, you need nutrients to support your energy demands, heal connective tissues and keep your energy levels as stable as possible. You may need to keep going for several hours without a break, so if you can maximise your food quality when you do get a chance to eat, the better you’ll be able to care for your baby.
If you are breastfeeding, you are your baby’s only source of nutrients. Breast milk is full of minerals your baby needs to grow, including iron, zinc, calcium, sodium, chloride, magnesium, and selenium[5]. These micronutrients are crucial for the development of healthy bones, producing red blood cells and promoting proper muscle and nerve function. Consuming a diet rich in high-quality proteins, healthy fats, and lots of vegetables is the main way you can ensure your baby receives everything he or she needs to grow.
One of the most crucial forms of nutrients your baby needs if you are breastfeeding is DHA, an omega-3 fatty acid found primarily in oily fish. 60% of the total energy in human milk is contributed by lipids, with 10-12% of that coming from essential fatty acids. These unsaturated fats are crucial to the development of your baby’s brain, nervous system and vision[6],[7].
We also know that the foods you choose through pregnancy and nursing have a significant impact on your child’s food preferences and health outcomes in later life[8],[9],[10]. Early exposure to certain foods, both through pregnancy and breastfeeding, helps positively influence your child’s acceptance of foods like green leafy vegetables[11].

Make protein the star of every meal
Proteins form the building blocks of muscle and tissue, so you will need to ensure adequate intake when your body is healing from a major trauma. An additional benefit of high protein intake is that it is highly satiating, meaning that it will keep you fuller for longer while you’re trying to juggle nappy changing, feeding, burping and generally being run off your feet. Protein also has the highest thermic effect of food, and around 20% of its calories are required for digestion. So, even though weight loss doesn’t need to be an immediate priority, high protein intake may indirectly help it.

Supplement where needed
While the bulk of your micronutrient intake should come from healthy dietary choices, there are some instances in which supplementation is useful and even essential. For most women, supplementing with folate and vitamin D3 is required to plug nutritional gaps. If you follow a plant-based diet, additional intake of iron, folic acid, B12 and omega-3 fatty acids is essential for ensuring your child’s healthy development.
Before you take any supplements, make sure to speak to your doctor or healthcare provider first.
Hydrate
Water accounts for nearly 75% of body weight in infants and 55% in elderly populations; it is crucial for maintaining homeostasis and nearly all physiological processes[12]. Human breast milk is also composed of around 90% water[13]. You don’t necessarily need to increase your water intake beyond normal, but because breast milk provides all your child’s water requirements, ensuring good hydration is key.

Aim for simple but effective
You don’t need to worry about being a super mum right now but keeping things simple will help you stay nourished for yourself and your baby, especially if you’ve only got one hand and minimal time available. Here are some tips to keep your nutrition stress free and time-efficient:
- Buy pre-prepared vegetables: frozen veg in microwave bags that will be ready in minutes, pre-chopped veg, such as carrots or root veg that can go straight in the oven, pre-chopped onions or mushrooms to add into bigger dishes.
- Make use of your slow cooker or steamer. Anything that’s a one-pan wonder is a great option for saving time and making multiple servings you can save for later.
- Buy pre-cooked/ pre-packaged proteins. Go for options like rotisserie chicken, peeled, boiled eggs, high-protein yoghurts in squeezy pouches.
- Keep healthy snacks at the ready. You might not always have time for a proper meal, so keep a few options around you can grab on the go. Nuts, berries, or even options like crudites are more filling than chocolate and will keep you going for longer.
Caffeine and breastfeeding
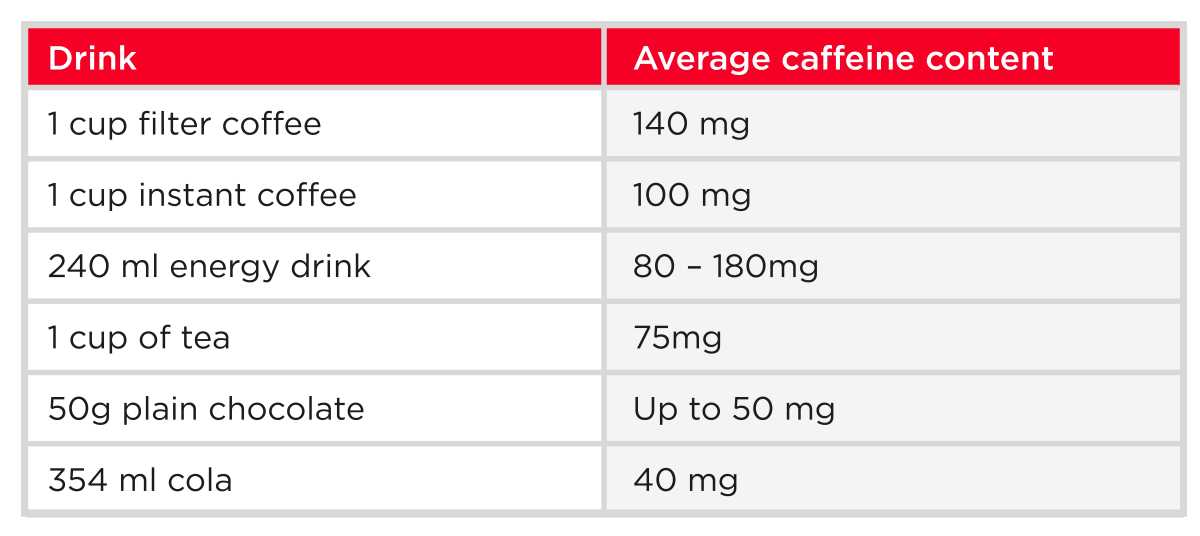
For as long as you’re breastfeeding, aim to minimise your caffeine consumption. This is because whatever you drink, so does your baby. Caffeine in babies can result in prolonged waking or agitation, which is probably the last thing you need![14] Try to restrict your total caffeine intake to no more than 200 mg per day[15]. Don’t forget that caffeine is also included in energy drinks, soft drinks, certain foods, and medications.
Where possible, opt for decaf versions of tea or coffee or herbal teas. Fruit juice is ok but limit yourself to one 150 ml glass per day[16].
Alcohol and breastfeeding
When it comes to alcohol while breastfeeding, the main thing to remember is that whatever you consume, so does your baby. However, in terms of strict guidelines on drinking, the message is less clear. In the US, the Institute of Medicine advises that women can drink 8 oz (236 ml) of wine, 12 oz (340 ml) of beer or a double shot of spirits (2oz) if they don’t breastfeed for a further two hours[17]. In the UK, guidelines state that you should minimise drinking to no more than 14 units per week, making sure to avoid feeding for two to three hours to prevent exposing your baby to any alcohol in your milk.
However, the research into how you need to wait before breastfeeding is again inconclusive. Expressing and pouring away milk, also known as ‘pump and dump’, relieves breast engorgement. The aim here is to stimulate the breakdown of alcohol rather than remove it from the milk altogether[18]. Eating a meal before drinking may reduce how much alcohol is available by up to 38% and if you pump beforehand, this number reduces further to 58%[19]. Other factors such as your baby’s age, your height and weight, genetics, and ability to metabolise alcohol also play a role. As a result, there are no clear-cut answers for how long it takes for your milk to reach the recommended level of zero alcohol.

The table above is adapted from a study that explored the amount of time required for breast milk to show zero alcohol content at different maternal weights after different amounts of alcohol intake[20].
Note that this study only examined how long it takes for alcohol in breast milk to reach zero levels without pumping; it did not compare alcohol levels with pumping against not pumping. However, it demonstrates the variability in rates of alcohol metabolism depending on factors such as weight. The key takeaway is that while you can drink alcohol in moderation while breastfeeding, it is important to plan your feeding schedule by expressing and storing milk in advance or waiting for the alcohol to completely clear from your system[21].
Lifestyle
Sleep
It’s safe to say that sleep is a major casualty when you have a new baby, who unfortunately doesn’t always sleep to schedule. The initial phase when your baby wakes several times a night doesn’t last forever. But in the meantime, here’s what you can do to maximise your sleep quality.
Nap when your baby sleeps
It’s incredibly common for women to experience shifts in sleeping patterns and sleep disturbances post-partum[22]. While it’s a cliché that you should nap while your baby sleeps, it’s common advice for a reason. It may be tempting to catch up on the pile of dishes in the sink or other chores, but every minute of rest you can get will help you navigate these challenging first few weeks.

Maximise your daylight exposure
Your circadian rhythm plays a crucial role in nearly every bodily process, and sleep is no exception. Light exposure is vital to regulating the body’s internal body clock, which signals when you should be alert and at rest. When exposed to natural light, your body synchronises with changes in light levels. While bright light in the morning increases cortisol and alertness, lower light through the afternoon and evening triggers the release of melatonin, causing you to feel sleepy. As a result, your natural sleep pattern is highly attuned to shifts in light levels.
In new-born infants, circadian rhythm develops postnatally, with cortisol rhythm beginning at around eight weeks, melatonin and sleep efficiency at nine weeks, and body temperature rhythm and circadian genes at eleven weeks post-partum[23]. Because babies need to feed frequently and have not yet developed circadian signalling, they are likely to wake you several times during the night.
However, the more daylight exposure you can get with your baby during the day, the better. Increased light exposure has been closely linked to the regulation of both sleep and mood in post-partum women and has also been linked to the improved establishment of normal circadian rhythm in infants[24],[25],[26]. Not only will it help you improve your sleep quality, it should also help your little one settle into a more sociable bedtime routine. If getting outside isn’t always possible, light therapy through tools like a SAD lamp in the morning for around one to three hours can also help improve circadian alignment[27].

Invest in blackout blinds or a blackout eye mask
Of course, sleeping on demand is not always easy, especially when you’ve been running around caring for a new-born! It’s very common for women to experience insomnia post-partum, and there is a strong correlation between sleep disturbances, fatigue and postnatal depression[28]. In particular, low sleep quality seems to be a significant risk factor for developing depressive symptoms[29]. Investing in blackout blinds or an eye mask is a simple trick that will improve your sleep quality, while white noise, like rain sounds or waves, can also help relax you in preparation for sleep.
Get out for a walk as often as you can
Not only is walking great for improving mental and physical health, but daily walking also appears to improve sleep quality[30]. Walking in nature has also been shown to be particularly effective at promoting mental well-being[31]. You don’t need to brace yourself for a full-on hike; simply getting out into some green space will provide benefits and maybe even some welcome quiet time.

Limit your caffeine intake
If you’re breastfeeding, you’re probably already limiting your caffeine intake anyway. However, if you drink caffeinated drinks, remember that caffeine takes around five hours to leave the system, so try to avoid it in the hours before sleep[32].
Don’t be afraid to reach out for support
They say it takes a village to raise a child, and that’s certainly true when it comes to sleep. Don’t be afraid to reach out to friends and family if you’re struggling to get enough rest or find yourself feeling frequently frazzled or low. If you have a partner, ask them to help with sharing feeds by expressing milk in advance once you’re in a good routine or ask them to help in the morning so you can go back to sleep. If you feel overwhelmed, don’t feel like you need to muddle through. Speak to your doctor or midwife, who will be able to direct you to relevant support services.

Read how new mum Lola overcame her diastasis recti to lose 15kg after pregnancy.
Stress management
Childbirth is a stressful event, and the changing shifts in your responsibilities, sleep patterns and lifestyle are certainly challenging. Levels of oestrogen, a hormone closely associated with antidepressant characteristics, may drop by more than 100% in the first three days after birth. This sharp hormonal decrease causes what is known as ‘baby blues’, when you may feel emotional, tearful, and more anxious or irritable than usual. Baby blues affects anywhere between 33-80% of women[33]. While these feelings should subside after around 10-14 days, if they persist or you experience ongoing feelings of overwhelm, reach out to your doctor or health visitor.
As manic as this time is, try not to let stress get the better of you. Here are a few tips to help you stay on top:
Don’t feel like you have to be superhuman
There’s a lot you’re trying to juggle right now, especially if this is your first child. Don’t stress about the housework if it’s a choice between you resting or doing chores. Giving yourself a breather to gather your thoughts will be far more beneficial in the meantime than trying to white-knuckle your way through.
Talk to those around you
Stats indicate that women are often afraid to reach out to others due to fear of judgment from family and friends[34]. Engaging in talking therapies such as detached mindfulness and stress management training have been shown to lead to significant and long-lasting improvements in women with postnatal depression[35].
Maximise your fibre intake and nutrient quality
High-fibre foods are essential for maintaining a healthy gut microbiome and the production of short-chain fatty acids, which your body uses to produce neurotransmitters such as dopamine and serotonin. You’ll likely find times where you’ll settle for the nearest thing you can lay your hands on, but the more often you can opt for high-quality fruit and veg, the greater the benefits for your mental health.
Keep moving
Studies into the occurrence of postnatal depression have found that active mums are less likely to develop depressive disorders in the postnatal period[36]. We all know that exercise releases a whole host of endorphins, but of course, there will be times when you feel so wiped out you don’t want to go anywhere or do anything. Even though you might not always feel up to it, keeping active will help lift your mood, even if you can only manage gentle exercise like walking.
Guided breathing
Guided breathing techniques have been consistently shown to stimulate the vagus nerve, which controls your parasympathetic (rest-and-digest) system, thereby promoting relaxation[37].
If it feels like everything is getting on top of you, try a couple of minutes of box breathing:
- While sitting, breathe in through your nose for a count of 4, taking the breath into your stomach.
- Hold your breath for a count of 4. Release your breath through your mouth with a whooshing sound for a count of 8.
- Without a break, breathe in again for a count of 4, repeating the entire technique 3-4 times in a row.
The take-home
There’s no doubt that a new baby brings many new challenges that make even the simplest of daily tasks seem like climbing Everest. But while you can’t control how much time and care your baby requires, focusing on some of the elements you can control may help you navigate the post-partum period. You don’t have to be ‘supermum’ but keeping active outdoors and maximising your nutrient intake from high-quality sources, is a major step in the right direction.
There will be many things that you don’t get right – don’t be afraid to reach out for support if you feel consistently overwhelmed, down, or overly tired. If you feel like you’re struggling, speak to your GP or get in touch with the resources below.
NHS. Overview – Postnatal depression
Pre and Postnatal Depression Advice and Support (PANDAS)
Association for Post Natal Illness (APNI)
References
[1] Russell, R. and Reynolds, F., (1997). Back pain, pregnancy, and childbirth: postpartum pain is most likely to be a continuation of antepartum pain. British Medical Journal, 314 (7087). [2] Koletzko, B., (2019). Nutrition during pregnancy, lactation and early childhood and its implications for maternal and long-term child health: The Early Nutrition Project Recommendations, Nutrition and Metabolism. 74 (2), pp. 93-106. [3] Fernandes da Mota, P.G., Pascoal, A.G., Carita, A.I., Bø, K., (2015). Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Manual Therapy. 20 (1), pp. 200-5. [4] Sperstad, J.B., et al. (2016). Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. British Journal of Sports Medicine. 50 (17), pp. 1092-6. [5] Dror, D.K., Allen, L.H., (2019). Overview of nutrients in human milk. Advances in Nutrition. 9 (supplement 1), pp. 278S–294S. [6] Crawford, M.A., et al. (1981). Essential fatty acid requirements in pregnancy and lactation with special reference to brain development. Progress in Lipid Research, 20, pp. 31-40. [7] Mazzocchi, A., D’Oria, V., De Cosmi, V., et al. (2018). The role of lipids in human milk and infant formulae. Nutrients. 10 (5), pp. 567. [8] Birch, L.L., Fisher, J.O., (1998). Development of eating behaviors among children and adolescents. Pediatrics, 101, pp. 539–49. [9] Rohlfs, D.P., (2011). Flavor exposure during sensitive periods of development as a key mechanism of flavor learning: implications for future research. American Journal of Clinical Nutrition. 93, pp. 909–10. [10] Harris G. (2008). Development of taste and food preferences in children. Current Opinion in Clinical Nutrition and Metabolic Care, 11, pp. 315–9. [11] Azagba, S, Sharaf, M.F. (2012). Fruit and vegetable consumption and body mass index: a quantile regression approach. Journal of Primary Care & Community Health, 3, pp. 210–20. [12] Nicolaidis. S., (1998). Physiology of thirst. In: Arnaud, M.J., ed. Hydration Throughout Life. Montrouge: John Libbey Eurotext, pg. 247. [13] Martin, C.R., Ling, P.R., Blackburn, G.L., (2016). Review of infant feeding: Key features of breast milk and infant formula. Nutrients. 8 (5), pg. 279. [14] American Academy of Pediatrics (2011). Bright Futures: Nutrition, third edition. AAP Publications. [15] NHS (2018). Breastfeeding and diet. https://www.nhs.uk/conditions/baby/breastfeeding-and-bottle-feeding/breastfeeding-and-lifestyle/diet/ [Accessed 09.11.2021]. [16] NHS (2018). Breastfeeding and diet. https://www.nhs.uk/conditions/baby/breastfeeding-and-bottle-feeding/breastfeeding-and-lifestyle/diet/ [Accessed 09.11.2021]. [17] American Academy of Pediatrics (2011). Bright Futures: Nutrition. [18] Pepino, M.Y., Mennella, J.A., (2008). Effects of breast pumping on the pharmacokinetics and pharmacodynamics of ethanol during lactation, Clinical Pharmacology & Therapeutics, 84 (6), pp. 710-714. [19] Pepino, M.Y., Mennella, J.A., (2008). Effects of breast pumping on the pharmacokinetics and pharmacodynamics of ethanol during lactation. [20] Ho, E., Collantes, A., Kapur, B.M., Moretti, M., Koren, G., (2001). Alcohol and breast feeding: calculation of time to zero level in milk. Biology of the Neonate. 80 (3), pp. 219-22. [21] Ho, E., Collantes, A., Kapur, B.M., Moretti, M., Koren, G., (2001). Alcohol and breast feeding: calculation of time to zero level in milk. [22] Hunter, L.P., Rychnovsky, J.D., Yount, S.M., (2009). A selective review of maternal sleep characteristics in the postpartum period. The Journal of Obstetric, Gynecologic, & Neonatal Nursing. 38 (1), pp. 60-8. [23] Yates, J., (2018). Perspective: The Long-Term Effects of Light Exposure on Establishment of Newborn Circadian Rhythm. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine, 14(10), pp. 1829-1830. [24] Barion, A., Zee, P.C., (2007). A clinical approach to circadian rhythm sleep disorders. Sleep Medicine. 8 (6), pp. 566-77. [25] Gallaher, K.G.H., Slyepchenko, A., Frey, B.N., Urstad, K., Dørheim, S.K., (2018). The Role of Circadian Rhythms in Postpartum Sleep and Mood. Sleep Medicine Clinics. 13 (3), pp. 359-374. [26] Yates, J., (2018). Perspective: The Long-Term Effects of Light Exposure on Establishment of Newborn Circadian Rhythm. [27] Chesson, A.L. Jr., Littner, M., Davila, D., et al. (1999). Practice parameters for the use of light therapy in thetreatment of sleep disorders. Standards of Practice Committee. American Academy of Sleep
Medicine Sleep. 22 (5), pp. 641–60.
[28] Hunter, L.P., Rychnovsky, J.D., Yount, S.M. (2009). A selective review of maternal sleep characteristics in the postpartum period. The Journal of Obstetric, Gynecologic, & Neonatal Nursing. 38 (1), pp. 60-8. [29] Posmontier, B., (2008). Sleep quality in women with and without postpartum depression. Journal Of Obstetric, Gynecologic, And Neonatal Nursing, 37 (6), pp. 722–737. [30] Wang, F., Boros, S. (2021). The effect of daily walking exercise on sleep quality in healthy young adults. Sport Sciences for Health. 17, pp. 393-401. [31] Gladwell, V., Kuoppa, P., Tarvainen, M., Rogerson, M., (2016). A lunchtime walk in nature enhances restoration of autonomic control during night-time sleep: results from a preliminary study. International Journal of Environmental Research and Public Health, 13, pg. 280. [32] Institute of Medicine (US) Committee on Military Nutrition Research. (2001). Caffeine for the Sustainment of Mental Task Performance. Washington (DC): National Academies Press (US). [33] Hopkins, J., Marcus, M., Campbell, S.B., (1984). Postpartum depression: A critical review. Psychological Bulletin, 95, pp. 498-515. [34] Dennis, C.L., Chung-Lee, L., (2006). Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 33 (4), pp. 323-31. [35] Ahmadpanah, M., Nazaribadie, M., Aghaei, E. et al. (2018). Influence of adjuvant detached mindfulness and stress management training compared to pharmacologic treatment in primiparae with postpartum depression. Archives of Women’s Mental Health, 21, pp. 65-73. [36] Kołomańska-Bogucka, D., & Mazur-Bialy, A. I. (2019). Physical activity and the occurrence of postnatal depression-a systematic review. Medicina. 55 (9), pg. 560. [37] Zaccaro, A.; Piarulli, A.; Laurino, M.; Garbella, E.; Menicucci, D.; Neri, B.; Gemignani, A. (2018). How Breath-Control Can Change Your Life: A Systematic Review on Psycho-Physiological Correlates of Slow Breathing.Frontiers in Human Neuroscience. 12, pg. 353.



