Are you concerned about infertility? While often considered a ‘female-only’ issue, statistics indicate that infertility affects an increasing number of men.
Several studies have reported decreases in sperm counts in Western countries over the last two decades, fuelled by environmental and lifestyle factors that result in reduced sexual function[1],[2],[3],[4]. The severity of the situation is such that experts have even suggested there is a male fertility crisis[5], [6].
However, the ramifications of this worrying trend go far beyond the ability to produce children. Infertility can be a source of great emotional distress and sadness, alongside the obvious repercussions for sexual relationships[7]. Male infertility, therefore, has significant implications for physical, mental and social health.
But there is good news: lifestyle changes significantly increase your chances of conception. In this second instalment in our men’s health series, we explore everything you need to understand what exactly happens down there, the main signs and symptoms of infertility, and actionable tips to improve your chances of starting a family.
What Is Male Fertility?
Male fertility (also known as fecundity) is a man’s ability to impregnate a woman and produce offspring. In clinical settings, infertility is defined in men and women when they cannot achieve pregnancy after one year of intercourse without birth control. Research indicates that around 15% of couples cannot conceive after this one-year mark, decreasing to 10% after two years[8], [9].

Male Infertility Statistics:
- An estimated 7% of all men are affected by infertility.
- Infertility affects around one in seven heterosexual couples in the UK.
- Generally, 30% of fertility problems are due to the man, 30% due to the woman, and 30-40% are due to both or unknown reasons.
- 10-15% of infertile men have a complete lack of sperm.
- In around half of male infertility cases, the cause is unexplained.[10]
Male Sexual Health: A Quick Biology Lesson
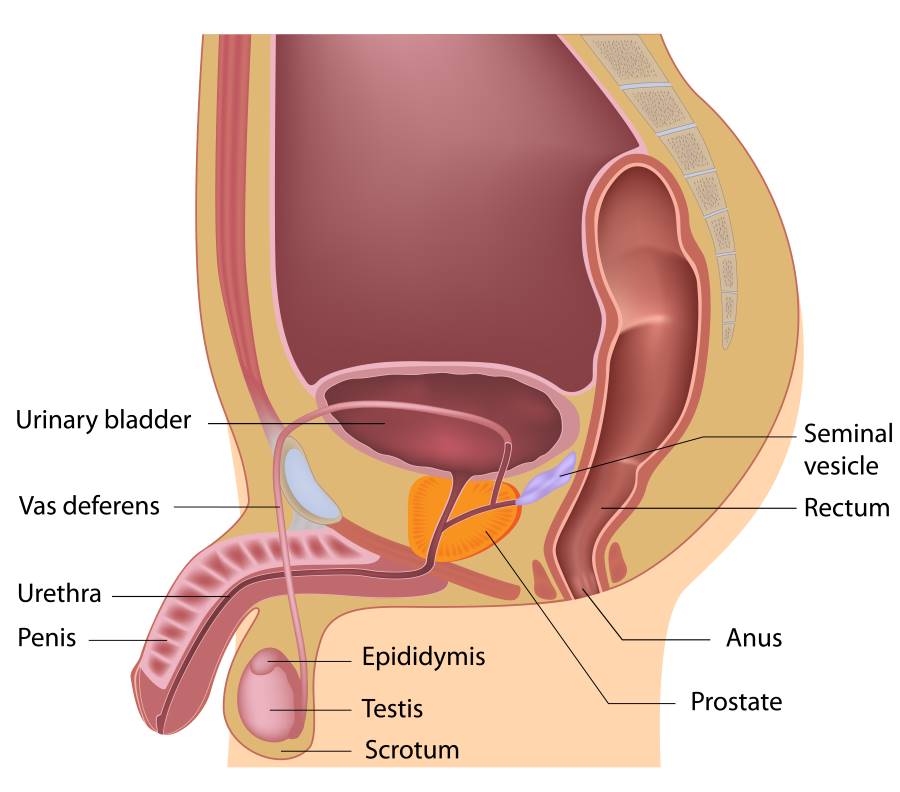
Under normal circumstances, the sperm must combine with the woman’s egg (ovum) to conceive. A man’s body makes tiny cells known as sperm, delivered into the woman’s body during sex via ejaculation. The male reproductive system consists of:
- The scrotum. A sack of skin below the penis that contains the testicles.
- The testicles. Two glands that sit in the scrotum and produce sperm and testosterone.
- The epididymis. A tube that sits behind each testicle, which carries the sperm from the testicles to another set of tubes called the vas deferens.
- Vas deferens. Each tube leads from the epididymis to behind the bladder in the pelvis. Each vas deferens joins the ejaculatory duct from the seminal vesicle. At ejaculation, the sperm mix with fluid from the prostate and seminal vesicles to form semen. The semen then travels through the urethra and out of the penis.
- The penis. The final piece of the puzzle delivers the sperm on ejaculation during sex to fertilise the egg.
Successful conception depends on every part of this chain functioning optimally. Once a man ejaculates, the sperm travel through the woman’s cervix into the uterus and fallopian tubes. If she has ovulated and produced an egg, fertilisation will happen when the sperm and egg meet. However, this is a delicate process and genes, hormonal levels and environmental conditions all need to be just right for the process to be successful.
What Causes Male Infertility?
Because conception is a complex process, numerous factors can impact male fertility. For example, the sperm may, for some reason, fail to reach the egg, or even the temperature of the scrotum may affect a man’s ability to conceive.
Multiple mechanisms affect male fertility, which may include:
- Inherited disorders.
- Hormonal imbalances – very low hormone levels cause poor sperm growth.
- Dilated veins around the testicles.
- Obstruction (conditions that block the passage of sperm).
- Immunological infertility (where a man’s antibodies attack his sperm).
- Medication. Certain medications can change sperm production, function and delivery. This includes medications used to treat:
- Arthritis.
- Depression.
- Digestive problem.
- Anxiety or depression.
- Infections.
- High blood pressure.
- Cancer.
Most commonly, infertility stems from problems producing sperm, which may include:
- Sperm not growing fully.
- Oddly shaped sperm (sperm morphology).
- Sperm not moving correctly (motility).
- Only producing sperm in very low numbers (oligospermia).
- Not producing sperm at all (azoospermia).
These issues can originate from genetic traits but lifestyle factors, such as alcohol consumption, smoking and medications, are major contributors. Damage to the delicate reproductive system can also inhibit sexual function. Around four in ten men who fail to produce sperm (azoospermia) suffer from an obstruction within the tubes that carry the sperm. Birth defects or infections can also be contributory factors[11].
Low testosterone (clinically referred to as hypogonadism) is a common cause of male reproductive issues, and research shows that as many as one in three infertile men meet the criteria for the condition[12].

Signs of Male Infertility
The most obvious symptom of male infertility is the inability to achieve pregnancy. However, because there are often no outward indications, many men remain unaware.
Male infertility may result in one or more of the following symptoms:
- Impaired sexual function, e.g. difficulty ejaculating, reduced volumes of ejaculate, low sex drive, and erectile dysfunction.
- Pain, swelling or lumps on the testicles.
- Recurrent respiratory infections.
- Loss of or reduced sense of smell.
- Growth of breast tissue (gynecomastia).
- Reduced/ difficulty growing facial hair or other indicators of hormonal imbalances.
- Reduced sperm count (fewer than 15 million sperm per millilitre of semen or a total sperm count of less than 39 million per ejaculate)[13].
When To See Your Doctor
If you have been unable to conceive after one year of regular, unprotected sex or if you experience any of the following symptoms, you should consult with your doctor:
- Erection or ejaculation problems, low sex drive, or other problems with sexual function.
- Pain, discomfort, a lump or swelling in the testicle area.
- A history of testicle, prostate or sexual problems.
- A groin, testicle, penis or scrotum surgery.
- You or your partner is over the age of 35.

Treatment
The causes and symptoms of male fertility may be multiple and complex, meaning that diagnosis can often be challenging. In most cases, if you’re worried about infertility, you should visit your doctor, who will be able to start blood work and further tests.
This will likely include:
1.Medical history and a physical examination.
A review of defects in your reproductive system, low hormone levels, sickness, or accidents. It could also include details of childhood illnesses, current conditions or medications, and exposure to recreational drugs or environmental toxins, like heavy metals.
2. Semen analysis.
Routine lab tests can help determine whether you are producing enough sperm and if they are functioning well. Your health care provider will study sperm volume, count, concentration, movement (motility) and structure (morphology). Low sperm count does not automatically mean that conception is an impossibility; it may simply be a problem with sperm growth or delivery.
3. Transrectal ultrasound.
An ultrasound that provides a detailed view of the male sexual organs and can indicate any physical problems.
4. Testicular biopsy.
5. Hormonal profile testing.
To determine whether your testicles are producing sperm. Follicle-stimulating hormone (FSH) is the pituitary hormone that tells the testicles to make sperm. High levels may mean your pituitary gland is trying to get the testicles to make sperm, but the testicles are non-responsive.

Lifestyle Changes
Consistent research shows that behaviour modification can make a significant difference to male fertility[14]. So, while the causes of male infertility are complex, improving your fertility isn’t entirely out of your control.
1. Lose Weight.
There are long-established links between obesity and male infertility, with obese men being 66% more likely to be infertile than healthy-weight men. One of the key mechanisms behind this is the impact of obesity on hormonal health, with as many as 64% of overweight men having low testosterone[15], [16]. However, it is more than possible to reverse this trend. Research in obese males has shown that shedding 15% of total body weight improves sperm quality and testosterone production[17]. Therefore, achieving a healthy body composition is one of the most important steps to boosting your chances of conception.
2. Make Smarter Dietary Choices.
Dietary choices appear to have a strong influence on male fertility. Men who consume a diet low in processed foods while high in vegetables, protein, and healthy fats, see significant improvements in their sperm quality and quantity[18]. Equally, studies show that phytoestrogens in soy products, such as tofu and soy milk, may impact testosterone production and sexual function. A study in Asian men found that free testosterone (the form the body can most easily use) dropped after consuming 60 mg of soy isoflavones for just six weeks[19]. That should be more than enough reason to ditch the soy milk!
3. Increase Your Activity Levels.
Inactivity is a major contributor to infertility. Studies show that sperm production decreases by as much as a third in inactive men, and sedentary lifestyles increase the risk of low testosterone by 50%[20]. On the flip side, exercising at least two to three times per week has proven benefits for sperm count, motility, and morphology, with intense exercise, such as resistance training, bringing the biggest improvements[21], [22].

4. Quit Smoking.
Smoking decreases sperm count and increases the risk of problems with sperm morphology[23]. While kicking the habit provides multiple other health benefits, it is crucial if you’re thinking about conceiving.
5. Manage Stress.
Stress has a major impact on male reproductive health. Chronic stress appears to decrease semen volume, as well as sperm motility and morphology[24]. Feelings of work-related stress, anxiety, and irritability can also signify low testosterone, a hallmark of infertility[25]. If you’re concerned about infertility, prioritising stress management through meditation or journaling.
6. Improve Your Sleep.
Sleep plays a pivotal role in general health and wellbeing but fertility especially. A recent observational study found that men who sleep for less than seven hours a night are more than six times more likely to produce abnormal sperm than men who sleep for eight hours or more[26]. One of the main ways you can improve your sleep is through improving your sleep hygiene, including keeping regular sleep and wake times, increasing your daylight exposure and avoiding blue-light-emitting devices in the hours before bed.

Think Carefully About Your Medications.
Some pharmaceutical medications, including treatments for depression, epilepsy, HIV antiretrovirals, and certain antibiotics, have links to decreased sperm quality and quantity[27]. Your medication history may provide important clues that can help pinpoint the cause of fertility issues.
The rising trend in recent years for hair transplants may have also contributed to the fertility crisis. Drugs such as finasteride, typically prescribed to support surgical interventions, may negatively affect male sexual health. Finasteride works by blocking an enzyme called type II 5α-reductase, responsible for converting the hormone testosterone into dihydrotestosterone (DHT). This results in increased testosterone levels and decreased levels of dihydrotestosterone, thereby encouraging the growth and retention of new hair.
However, this does not come without concessions. The use of finasteride may induce multiple sexual side effects, such as erectile and ejaculatory dysfunction and loss of libido[28]. Such effects appear to cease after continuous use of the drug or stopping altogether, but the jury is still out regarding whether such interventions cause long-term issues. However, if you’re trying for a baby, it may be wise to leave the trip to the surgeon until after you’re done having children.
Care For Your Assets.
Direct trauma to the testes, such as severe physical impact, long-distance cycling or even remaining seated for extended periods, can reduce sperm count, semen volume, and sperm quality[29]. Be mindful also of tight-fitting underwear and clothing as the testes sit outside of the body for a reason: temperatures that exceed natural limits have proven negative effects on sperm quality[30],[31]. To give yourself the best chance of conceiving, throw out the tight Y-fronts and skinny jeans.
Summary
Male infertility is a complex issue that has wide-ranging implications for physical, emotional and social health. It’s impossible to pinpoint the cause without expert medical investigation, so you should visit your doctor if you are concerned about any of the points raised. However, if you want to improve your chances of conception, lifestyle and behavioural changes are within your control, and small efforts add up to big improvements.
Key Takeaways
- Physiologically, male fertility describes a man’s ability to impregnate a woman.
- Male infertility is a rising male health concern, which has grown in prevalence due to modern lifestyles and behaviours.
- The causes of infertility are wide, complex and require medical testing – if you’re concerned about your fertility, visit your doctor.
- Despite the physiological complexities of infertility, lifestyle changes are the number one change within your control to improve your chances of conception.
- Quitting smoking, improving your body composition through diet and exercise, and managing sleep and stress are all factors that will elicit positive change.
Zinc and Vitamin D3 have been shown to naturally increase levels of the luteinising hormone (the natural hormone in men that tells your body to make its own testosterone). Visit our Supplement Store to find out more about how taking these supplements can improve fertility.



