Women are increasingly leaving childbearing until later in life as a result of modern lifestyle changes and shifting societal attitudes.
Combined with the impacts of the modern Western diet and behaviours, this has led to a ‘fertility crisis’ in many developing countries.[1].
While age brings an unavoidable decline in fertility for women, lifestyle choices also play a critical role.
Read on to learn the steps you can take to protect and promote your fertility.
What Is Female Fertility and Why Does It Matter?
Female fertility is a woman’s biological ability to conceive a child, which decreases with age. For both men and women, the start of their fertile years is marked by the onset of puberty. In women, this takes place when she starts menstruating. While many assume that women remain fertile until menopause, infertility may begin around five to 10 years before this time[2]. Typically, infertility is the inability to conceive after one year of frequent, unprotected sex, or at least six months in women over 35[3].
And it’s important to note that fertility isn’t only important if you want children. Menstrual cycle disruptions, such as amenorrhea (losing your period for 90 days or more) and oligomenorrhea (an irregular or delayed menstrual cycle), can be signs of hormonal imbalances that significantly negatively affect the body.
So, whether or not you’re planning on starting a family, fertility is an important health marker.
What Affects Fertility in Women?
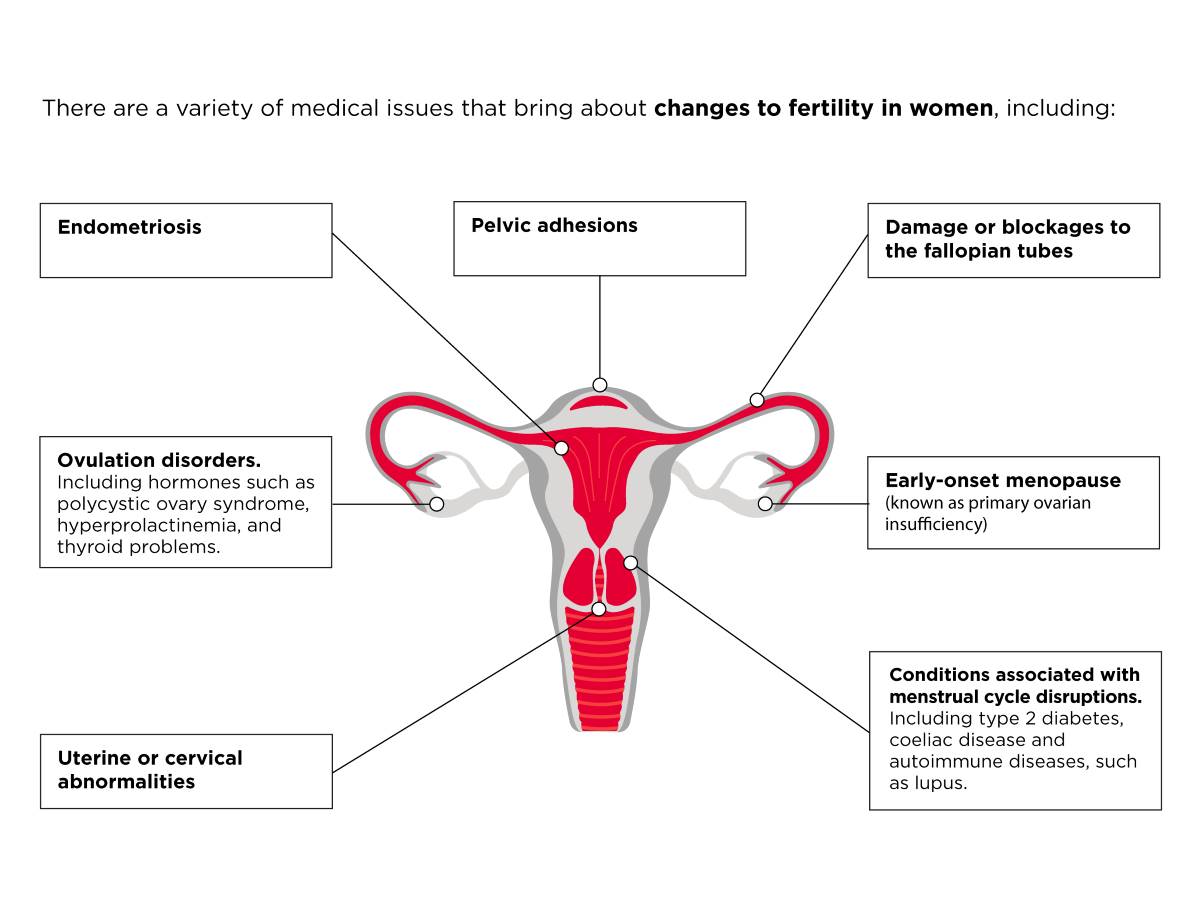
There are a variety of medical issues that bring about changes to fertility in women, including:
- Uterine or cervical abnormalities, including uterine polyps or fibroids.
- Damage or blockages to the fallopian tubes, often the result of pelvic inflammatory disease.
- Early-onset menopause (known as primary ovarian insufficiency). This occurs when the ovaries shut down, and menstruation ends under the age of 40.
- Ovulation disorders, which typically affect how the ovaries release follicles. This category includes hormones such as polycystic ovary syndrome (PCOS), hyperprolactinemia, and thyroid problems (hyperthyroidism or hypothyroidism).
- Endometriosis, a condition that affects around 6-10% of women[4]. It is a condition that causes the tissue lining the inside of the uterus to grow elsewhere.
- Many medical conditions are associated with menstrual cycle disruptions, such as type 2 diabetes, coeliac disease, and autoimmune diseases, such as lupus.
- Pelvic adhesions. The development of bands of scar tissue in the reproductive organs following pelvic infection, appendicitis, or abdominal or pelvic surgery.
Fertility and the Menstrual Cycle
A crucial factor regulating female fertility is the effective functioning of the menstrual cycle. Women are born with around one million egg-containing follicles, which number around 300,000 by the time she hits puberty. A woman only ovulates around 300 eggs throughout her reproductive years, one being released during each menstrual cycle. The remaining follicles are lost through the degenerative process known as atresia, which occurs regardless of external factors.
Each month, the pituitary gland releases a hormone known as follicle-stimulating hormone (FSH). This hormone causes a group of egg-containing follicles to grow on both ovaries. One follicle matures and releases an egg, known as ovulation. The remaining follicles degenerate. If sexual intercourse occurs during this time, known as the ‘fertile window’, and a sperm successfully fertilises the egg, it implants in the lining of the uterus. If this doesn’t happen, the lining or endometrium breaks down, sheds through menstruation, and the cycle repeats.
Under normal conditions, menstruation should occur over a 28-32-day cycle. However, it’s not unusual for it to last up to 40 days as this delicate process can become disrupted by various external and internal factors. Menstruation typically becomes shorter as a woman reaches her late thirties through to her early forties; ovulation may become more erratic and her periods less frequent. When a woman has not had a period for at least one year, she is deemed to have entered menopause.

Ageing And Female Fertility
Unfortunately, while male sperm counts decline with age, men retain the ability to produce offspring for most of their lives. In contrast, women face a monthly decrease in their ability to conceive as they release and lose multiple follicles. A woman’s most fertile years are in her twenties, with fertility beginning to decline gradually after thirty, particularly after 35. As a result, each month a woman tries to conceive, she has around a 20% chance of conception, which decreases to less than 5% per cycle by age 40[5].
Egg Quality
Ageing also has a significant effect on egg quality. This is because egg quality declines as a woman’s remaining number of eggs decreases. This becomes acute as she reaches her mid-to-late thirties.
Another important factor in egg quality is the occurrence of genetic abnormalities, known as aneuploidy, where a chromosome has too few or too many chromosomes. A normal egg has 23 chromosomes, which, when fertilised with a sperm with 23 chromosomes, produces an embryo with 46 chromosomes. With age, the number of eggs with the correct number of chromosomes decreases, increasing the risk of conditions like Down’s syndrome when the embryo has an extra chromosome. Embryos that have too few or too many chromosomes often result in no pregnancy or miscarriage.
Egg Quantity
A woman’s pool of follicles decreases in size with age, known as ‘loss of ovarian reserve’. This ovarian reserve begins to decline before women become infertile and before regular periods cease. Alongside this drop in ovarian reserve, a woman’s follicles become less sensitive to follicle-stimulating hormone (FSH). They therefore become less able to consistently ovulate, creating long, irregular cycles, as is often seen during perimenopause. In addition to age, other risk factors for loss of ovarian reserve include smoking, family history of premature menopause, and ovarian surgery.

Obesity and poor body composition are commonly linked to fertility problems in women.
Lifestyle Factors and Female Fertility
While ageing brings declines in fertility, behaviour and lifestyle are also significant contributing factors. This includes:
Obesity
Obesity and poor body composition are commonly linked to fertility issues and complications during pregnancy. A common dominator in obesity and fertility problems is polycystic ovary syndrome (PCOS), a hormonal imbalance affecting both health and appearance. PCOS affects around 15-20% of infertile women and is often associated with weight gain and obesity, specifically excess abdominal fat[6]. Obesity is a major contributing factor in PCOS, with 44% of obese women having PCOS compared with 9% of those of normal weight[7].
Sexually Transmitted Infections
Sexually transmitted infections, such as chlamydia and gonorrhoea, are preventable yet serious causes of pelvic inflammatory disease (PID) and infertility. Left untreated, 10-15% of women who contract chlamydia will develop PID. Chlamydia is often symptomless and can cause infections in the fallopian tubes. Both types of infections can also cause permanent damage to the fallopian tubes, uterus and surrounding tissues, resulting in infertility[8].
Working Patterns
Women under 35 who regularly work night shifts are more likely to require fertility treatment and experience menstrual irregularity or endometriosis, regardless of lifestyle factors and ethnicity[9]. It is thought that this could be caused by a disruption to the body’s natural circadian rhythm, which regulates most physiological processes.
Smoking
Cigarette smoking appears to have a chronic and dose-dependent adverse effect on ovarian function. Studies have found that women who smoke have a 50% reduced implantation rate and ongoing pregnancy rate compared with those who have never smoked. However, women who quit tend to see their fertility rates return to levels similar to those found in non-smokers[10].
Dietary Choices
Evidence indicates that diet has a critical impact on healthy hormonal functioning. Researchers have found that the quality and quantity of dietary carbohydrates impact glucose management and insulin sensitivity, affecting ovarian function and androgen production[11]. Intake of trans fats also appears to be related to higher risks of ovulatory infertility and endometriosis, although the findings are not conclusive[12]. Nonetheless, dietary patterns rich in whole grains, fruits, vegetables, and sources of monounsaturated and polyunsaturated fats, such as olive oil and oily fish, appear to improve the chances of pregnancy[13].

Diet is key to healthy hormonal functioning for women.
When To Refer Out
Around 80% of couples where the woman is under 40 conceive within the first year if they have regular intercourse without contraception. Cumulatively, this rate rises to 90% as around half who do not conceive within the first year do so in their second year of trying[14]. If you have been having regular, unprotected sex for at least a year, or at least six months if you’re over 35, with no success, it may be time to refer out. Equally, if you don’t have a regular cycle, sexual dysfunction, such as loss of libido, a history of pelvic disease or prior surgery, seek further advice as soon as possible.
Treatment Options for Infertility in Women
Female fertility tests include ovulation detection and analysis of the fallopian tubes, cervix and uterus, alongside a sperm test for the male partner. This process generally lasts around six months.
If you have a medical diagnosis of high blood pressure or type 2 diabetes, consult with your healthcare provider before trying to conceive, as you may be at increased risk of complications or require a change in medication.
Generally speaking, depending on the cause of infertility, treatment options may include assisted reproductive technologies, such as intrauterine insemination (SO/IUI) or in vitro fertilisation (IVF). For women over 40, the chances of success significantly increase with the use of donor eggs. This is because, by the age of 43, the chances of conception through IVF drop to 5%, with donor eggs becoming the only viable alternative by the age of 45[15].

Improving Fertility
While fertility is affected by various non-modifiable factors, lifestyle change can go a long way to improving your chances of conception.
1. Boost your physical activity levels
Research shows that sedentary women are three to four times more likely to become infertile[16]. However, regular exercise in overweight, obese, and sedentary women improves hormonal function and boosts conception rates[17]. Resistance training is also one of the most effective ways to improve fertility[18].
2. Eat a balanced diet and minimise alcohol
Dietary choices are a modifiable factor that significantly impacts pregnancy outcomes, from conception to birth and beyond. Micronutrient intake appears to improve the chances of conception and successful pregnancy, with folic acid, iron, and vitamin D all having proven benefits[19],[20]. While a balanced diet that includes plenty of fibre, high-quality fats and vegetables should be your baseline, this is an area where supplementation can help plug any gaps.
Likewise, if you are trying to conceive, consider cutting down on alcohol as women who regularly drink excessively are around 60% more likely to struggle than those who do so moderately[21].
3. Improve your body composition
Obese women are more than three times as likely as healthy-weight women to develop ovulatory infertility[22]. However, even relatively small amounts of weight loss (5-10% of total body weight) appear to improve health markers and fertility, alongside relative improvements in insulin sensitivity and physiological changes[23].
4. Manage stress
Stress of any kind can negatively impact your ability to conceive. Women who regularly experience high psychological stress see a two-fold increase in the likelihood of menstrual cycle dysfunction[24]. It’s important to note that professional mental health treatment appears to improve reproductive function[25].
Physical stress can cause what is known as functional hypothalamic amenorrhea (FHA) when the hypothalamus shuts down the menstrual cycle. It can occur due to high amounts of intense, strenuous exercise, harsh dieting, or reaching super-low levels of body fat (e.g., 10% body fat and lower). If this occurs for an extended period, a woman’s menstrual cycle becomes more likely to become disrupted. So, while it’s important to achieve a healthy body composition, make sure to prioritise your hormonal health also.
5. Quit smoking
Smoking is associated with a 60% increased risk of infertility in women, including an increased likelihood of lower sex hormones, such as progesterone[26],[27]. There are many benefits to quitting, but it is even more crucial if you’re thinking of trying for a baby.
6. Prioritise your sleep quality and quantity
Sleep has an often-overlooked impact on fertility, and women who sleep for less than seven hours are 15% more likely to be infertile[28]. In addition, insomnia, a common sleep disorder, is linked to a two-fold increase in menstrual cycle irregularity[29]. Regular sleep and wake times and daylight exposure are two key ways you can improve circadian rhythm regulation.

Improving your body composition can help improve health markers and fertility.
While medical advances in recent decades have meant that women can start families later than ever before, unfortunately the clock is still an important factor in female fertility. While age may not be something you can control, it is possible to improve your chances of conception through lifestyle choices. If you have concerns about your fertility or experience an irregular menstrual cycle, consult your health care provider, who can help you explore your options.
Key Takeaways
- Female fertility relates to a woman’s biological ability to conceive a child, which decreases as she ages.
- A woman is born with all her eggs, which decrease in number and quality over time.
- Difficulty conceiving can originate from problems with sexual organ function, hormonal dysfunctions, medical conditions, and, increasingly, lifestyle factors.
- Refer out if you are unsuccessful in conceiving after one year of consistent, unprotected sex or after six months if you are over the age of 35.
- There is a range of means of treating infertility in women. Your healthcare provider is best placed to discuss your options.
- While there are various non-modifiable risk factors for infertility in women, lifestyle and behaviour change are key to increasing the chances of conception.



